📌 The hidden reason your skin keeps burning down there

Posted 5 December 2025 by: Admin
Common Groin Irritations: Identifying The Culprits
The groin’s warm, moist, and confined environment creates the perfect breeding ground for skin problems. Unlike other body areas, this delicate region faces constant friction, perspiration, and exposure to irritants—making it particularly vulnerable to five distinct conditions that plague millions. Each stems from surprisingly common daily habits: the razor you use, the underwear you choose, or even the soap in your shower.
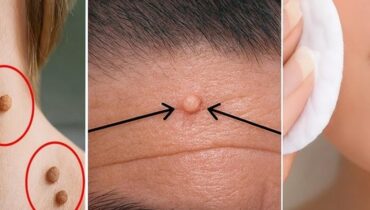
Ingrown hairs emerge when normal grooming practices go awry. Shaving, waxing, or plucking too closely forces hair to curl back into the skin, creating small red bumps that often become infected with pus. Tight clothing compounds this problem by increasing friction against newly shaved skin. Meanwhile, folliculitis presents as tiny red or white-headed pimples caused primarily by Staphylococcus aureus bacteria—commonly introduced through shaving wounds or unsanitary conditions. The distinction matters: while ingrown hairs result from mechanical irritation, folliculitis indicates active bacterial colonization.
Fungal infections add another layer of complexity. Tinea Cruris, commonly known as jock itch, thrives specifically in the groin’s moisture and warmth, spreading across inner thighs and buttocks. Contact dermatitis, conversely, springs from allergic or irritant reactions to everyday products: perfumed soaps, synthetic fabrics, latex, or even laundry detergent residue. Finally, intertrigo develops silently in skin folds where friction combines with trapped moisture and poor air circulation.
Understanding these distinct culprits proves essential because misidentification leads to ineffective treatment and prolonged discomfort.
The Warning Signs Your Body Is Sending
Distinguishing between these five conditions requires attention to specific visual and sensory markers. While they share a common location, each produces characteristic symptoms that serve as diagnostic clues—if you know what to observe.
Ingrown hairs and folliculitis often appear similar at first glance, yet their differences reveal their origin. Ingrown hairs present as small round bumps, frequently containing pus, accompanied by localized redness and intense itching. Folliculitis manifests as tiny red or white-headed pimples clustered around hair follicles, with tenderness extending to the surrounding skin. The bacterial nature of folliculitis typically causes mild burning alongside itching, distinguishing it from the mechanical irritation of ingrown hairs.
Jock itch displays unmistakable characteristics: red, scaly patches with sharply raised edges that gradually spread across the groin, inner thighs, and buttocks. The itching intensifies with moisture and heat, worsening throughout the day. Intertrigo similarly affects skin folds but produces raw, burning skin with a distinctive unpleasant odor—a telltale sign of trapped moisture and secondary bacterial growth. Contact dermatitis, by contrast, triggers widespread itchy and inflamed skin with potential peeling or blistering, usually appearing shortly after exposure to a new soap, detergent, or fabric.
These symptom patterns matter profoundly. They determine whether you’re dealing with a straightforward mechanical problem requiring simple prevention, a bacterial infection demanding antibacterial intervention, or a fungal condition necessitating specialized antifungal treatment. Accurate identification accelerates recovery and prevents unnecessary trial-and-error approaches that waste time and compound frustration.
Immediate Relief: Proven Treatment Protocols
Once you’ve identified which condition afflicts you, targeted treatment accelerates healing and prevents escalation. Each groin irritation responds to specific therapeutic approaches—attempting generic remedies wastes precious time and often worsens inflammation.
Ingrown hairs and folliculitis respond well to initial self-care measures. Apply warm compresses to reduce swelling and soften surrounding tissue, then gently exfoliate with specialized cleansers to release trapped hairs. For folliculitis specifically, antibacterial soap followed by topical antibiotic ointments addresses the bacterial component. Avoid shaving until complete healing occurs; resuming too early reintroduces the mechanical trauma that triggered the problem. Severe or recurring cases warrant professional extraction and oral antibiotics to eliminate persistent infection.
Fungal infections demand antifungal precision. Jock itch responds reliably to over-the-counter creams containing clotrimazole or terbinafine applied directly to affected areas. Intertrigo requires dual intervention: antifungal or talcum powders to absorb moisture, combined with barrier creams containing zinc oxide to prevent skin-to-skin friction. Secondary bacterial infections occasionally complicate intertrigo, necessitating concurrent antibacterial treatment.
Contact dermatitis improves dramatically once you identify and eliminate the offending substance. Switch to fragrance-free products and gentle moisturizers. Hydrocortisone cream effectively suppresses itching during the acute phase. The inflammation typically subsides within days of removing the irritant, distinguishing contact dermatitis from more persistent fungal or bacterial conditions that require sustained treatment intervals.
Moisture control remains universal across all conditions—the groin’s naturally humid environment perpetuates every listed irritation.
Prevention Strategies And Red Flags
Preventing groin irritation proves far more effective than managing recurring flare-ups. The foundation rests on deliberate daily habits that contradict the warm, moist environment where these conditions flourish.
Shaving technique and fabric choice form your first defense line. Always shave in the direction of hair growth using clean razors—this prevents hairs from curling back into the skin. Prioritize cotton underwear over synthetic materials; breathable fabrics allow moisture to escape rather than accumulate against vulnerable skin. Tight clothing intensifies friction and traps heat, accelerating irritation onset. After physical activity or sweating, change into dry clothes immediately and bathe promptly rather than allowing moisture to linger.
Hygiene extends beyond basic cleaning. Dry thoroughly after washing, particularly within skin folds where moisture pools. Never share razors, towels, or personal clothing items—these vectors efficiently transmit fungal and bacterial infections between individuals. Use fragrance-free soaps and lotions; unnecessary additives trigger contact dermatitis in susceptible skin.
However, even meticulous prevention occasionally fails. Recognize warning signals demanding professional intervention: rashes persisting beyond two weeks indicate established infection requiring targeted medication. Severe pain, pronounced swelling, or purulent discharge suggest bacterial complications needing oral antibiotics. Fever or flu-like symptoms signal systemic involvement. Rapidly spreading rashes that expand despite home treatment reveal infections resistant to over-the-counter approaches. These red flags transform a manageable condition into a medical priority requiring immediate dermatological assessment.