📌 Sudden prominent veins: 6 common benign causes and 3 warning signs that require an urgent consultation
Posted 1 January 2026 by: Admin
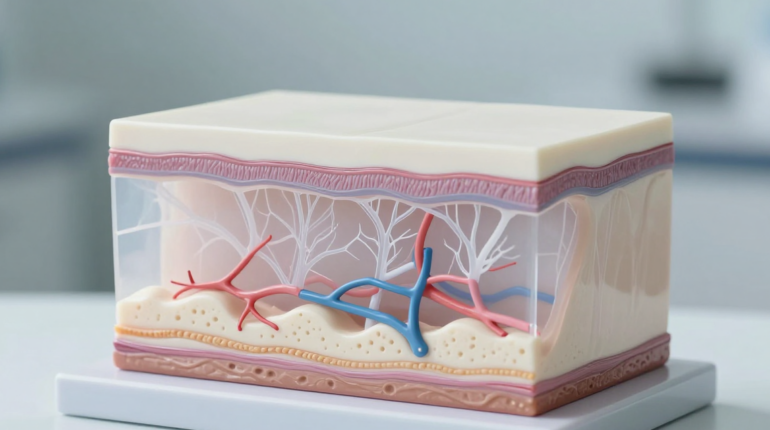
The Physiological Mechanisms Of Venous Appearance
The sudden emergence of prominent veins on the hands, arms, or legs finds its explanation in the very mechanics of our anatomy. The reduction of subcutaneous fat is the most common cause of this phenomenon: this fatty layer acts as a natural camouflage for the superficial venous network. Significant weight loss, a naturally thin constitution, or age-related fat redistribution are enough to reveal these previously invisible vessels.
Physical activity also plays a determining role. Exercise causes an increase in cardiac output and dilates veins to accommodate increased blood volume. In the long term, strength training develops muscle mass which literally pushes superficial veins toward the skin surface, creating that characteristic veiny look of athletes.
Thermoregulation temporarily amplifies this phenomenon: environmental heat, fever, or a simple hot shower trigger vasodilation of superficial vessels to evacuate body heat. Skin aging, with its progressive loss of collagen and elastin, makes the skin thinner and more transparent, further exposing underlying structures.
Hormonal fluctuations are a misunderstood but significant factor. During pregnancy, menopause, or certain hormonal treatments, variations in estrogen and progesterone modify vascular tone and blood volume, favoring the appearance of spider veins. Finally, genetic predisposition remains determining: hereditary venous elasticity and skin transparency transmitted by parents explain why certain families systematically present visible veins.
Medical Warning Signs Not To Ignore
While these physiological mechanisms explain the majority of cases, certain venous manifestations impose immediate vigilance. The sudden and unilateral appearance of prominent veins on a single limb, without an obvious trigger like new physical activity or weight loss, constitutes the first warning signal. This asymmetry suggests a localized obstruction or a change in vascular pressure that goes beyond the scope of simple physiological variation.
Superficial thrombophlebitis manifests as a vein that is firm to the touch, cord-like, accompanied by marked tenderness, redness, and local heat. This blood clot in a superficial vein, although less serious than deep vein thrombosis, requires medical evaluation to prevent any extension.
Deep vein thrombosis represents an absolute emergency. Although the clot itself remains invisible deep down, its consequences are seen on the surface: sudden swelling of a leg, intense pain evoking a persistent cramp, heat, and redness. Paradoxically, superficial veins can become more apparent, serving as bypass routes in the face of deep blockage. This situation requires immediate management, as the risk of pulmonary embolism imposes intervention without delay.
The combination of new venous visibility and inflammatory symptoms distinguishes benign change from vascular pathology. Pain, swelling, redness, or heat transform a simple anatomical observation into a clinical alarm signal.
Chronic Venous Insufficiency And Its Manifestations
Beyond vascular emergencies, chronic venous insufficiency sets in progressively, drawing a subtle line between normality and pathology. This deterioration of venous return results in visibly dilated and tortuous superficial veins, forming those familiar varicose veins that affect nearly 30% of the adult population.
The first clues go beyond simple aesthetics. Persistent heaviness in the legs at the end of the day, ankle edema that worsens with prolonged standing, and that sensation of skin tension reveal a venous system struggling to perform its function of returning blood against gravity. The skin itself bears witness to this vascular suffering: brownish pigmentation around the ankles, areas of venous eczema, and sometimes skin hardening reflecting chronic inflammation of poorly irrigated tissues.
At-risk populations include people in sedentary jobs or those involving prolonged standing, women who have had several pregnancies, and those with a family predisposition. Obesity and smoking significantly worsen this evolution.
Untreated, CVI progresses toward serious complications: venous ulcers that are difficult to heal, recurrent skin infections, or even repeated superficial thromboses. This evolutionary trajectory justifies early intervention, long before the appearance of these irreversible complications that lastingly compromise quality of life and require heavy treatments.
When To Consult: Informed Decision Criteria
Faced with this insidious progression, the crucial question remains: when to cross the threshold of the medical office? The answer rests on a clear prioritization of symptoms.
An urgent consultation is required without delay in the presence of acute pain associated with unilateral leg swelling, localized heat with redness, or suddenly cord-like and painful veins. These manifestations suggest a thrombosis requiring immediate management to prevent pulmonary embolism.
Conversely, veins that have become visible after significant weight loss or an intensive training program, without pain or edema, fall under simple monitoring. A scheduled consultation becomes relevant if persistent heaviness, repeated nocturnal cramps, or progressive skin changes are added.
The medical evaluation relies on venous echo-doppler, a non-invasive examination precisely mapping blood flows and detecting obstructions or pathological reflux. Depending on the results, therapeutic options range from medical compression and lifestyle modifications (regular physical activity, nocturnal leg elevation, adequate hydration) to targeted interventions: sclerotherapy for small varicose veins, thermal ablation, or surgery for severe cases.
Daily prevention remains fundamental: avoid prolonged immobile standing, prioritize walking which activates the calf muscle pump, maintain a healthy weight, and hydrate correctly. This vigilance transforms a suddenly visible venous network into a simple physiological reminder rather than a persistent medical concern.




















