📌 Your Nose Can Detect Death Before It Happens – Scientists Finally Explain How
Posted 3 December 2025 by: Admin
The Science Behind Smelling Death: When Our Nose Detects The Inevitable
The human body operates as a sophisticated communication system, constantly broadcasting signals that most of us remain oblivious to. Yet beneath this apparent silence lies a remarkable biological phenomenon: our olfactory system’s capacity to detect approaching death before conscious recognition arrives. Anecdotal accounts have long suggested that certain individuals perceive a distinctive odor preceding a loved one’s passing—experiences that hint at an extraordinary sensory awareness tied directly to our sense of smell.
Scientific investigation reveals plausible explanations for this mysterious perception. As the body approaches its final stages, it produces specific chemical compounds and odors imperceptible to most people. Some individuals, particularly those with heightened olfactory sensitivity, may unconsciously detect these subtle shifts. An alternative theory proposes that our olfactory system connects to deeper emotional processing, allowing us to sense imminent loss through channels we cannot fully explain.
Research from the University of Chicago provides compelling evidence. Scientists demonstrated that animals—dogs and cats—reliably detect chemical changes in individuals with certain medical conditions, including cancer. This finding suggests that humans with exceptional olfactory acuity possess similar capabilities. Hospital studies document remarkable instances where resident animals consistently and accurately predict patient deaths, sometimes days in advance.
These observations challenge our conventional understanding of how information travels through our senses. The olfactory system operates independently from our conscious awareness, processing molecular data that bypasses rational thought entirely. This mechanism may explain why individuals report “sensing” death without identifying a specific smell—their bodies recognized what their minds could not articulate.
Loss Of Smell As A Health Predictor: The Early Warning System
While the body’s capacity to broadcast death signals externally remains largely enigmatic, an equally compelling discovery emerges from the opposite direction: our own olfactory decline often precedes grave health consequences. The loss of smell operates as nature’s early warning system, signaling systemic deterioration long before clinical symptoms manifest.
Research demonstrates that declining olfactory function correlates strongly with neurodegenerative diseases. Parkinson’s and Alzheimer’s patients frequently experience smell loss years before cognitive or motor symptoms appear, suggesting the olfactory system’s heightened vulnerability to neurological damage. Beyond the brain, smell loss also indicates respiratory and cardiovascular compromise—organs equally critical to survival.
A landmark study published in the Journal of the American Geriatrics Society revealed striking evidence: elderly individuals with diminished sense of smell were significantly more likely to die within five years compared to those maintaining healthy olfaction. This finding transforms smell from a peripheral sense into a measurable mortality indicator, offering healthcare professionals and individuals themselves a concrete diagnostic opportunity.
The olfactory system’s deterioration pattern holds particular significance because it occurs invisibly, during the asymptomatic window when intervention remains most effective. Unlike visible disease progression, smell loss demands active awareness—patients must recognize and report this subtle shift to healthcare providers. This recognition gap underscores an uncomfortable reality: we remain largely unprepared to interpret the signals our bodies continuously transmit, even when science has decoded their meaning.
The End-Of-Life Timeline: Physical And Emotional Changes From Weeks To Final Moments
As awareness grows regarding smell’s role in predicting mortality, attention naturally shifts to what occurs during the final chapter itself. The dying process follows a remarkably consistent pattern, offering caregivers and loved ones a map through unfamiliar terrain. Understanding this timeline transforms confusion into recognition, fear into preparedness.
In the weeks preceding death, the body initiates its gradual shutdown. Emotional withdrawal mirrors physical decline—individuals often detach from daily life, lose interest in activities, and increasingly focus on memory. Appetite vanishes, weight drops noticeably, and fatigue becomes overwhelming. This phase demands patience rather than intervention; forcing food or engagement contradicts the body’s natural progression.
Days before the end, changes accelerate dramatically. Sleep dominates waking hours. Breathing becomes labored and irregular. Swallowing fails, confusion sets in, and some individuals experience hallucinations—conversations with absent loved ones or vivid perceptions others cannot share. Hearing, remarkably, remains intact until the final moments, making gentle speech and presence profoundly meaningful even when response seems impossible.
In the final hours, the body visibly surrenders. Breathing grows sparse and shallow, punctuated by extended pauses. Extremities cool; skin develops mottled patterns. The pulse weakens to imperceptibility. Yet consciousness may flicker—sudden clarity or brief awakenings offering final windows for connection.
When death arrives, vital functions cease completely. The body fully relaxes, eyes dilate without response, and skin turns pale and waxy. This timeline, while universal in structure, remains deeply individual in pace and manifestation, requiring caregivers to observe with compassion rather than rigid expectation.
Caring For The Dying: Essential Comfort Measures And Caregiver Support
As the end-of-life timeline unfolds with its predictable progression, the focus shifts toward what matters most—creating an environment where dignity, respect, and love define the final chapter. Comfort care during this phase transcends medical intervention; it becomes an act of profound presence and compassion.
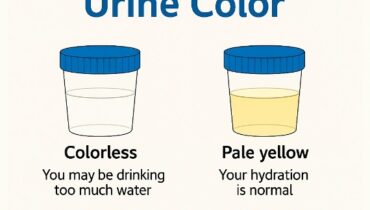
Physical comfort requires deliberate attention to basic needs. Hydration and skin care take priority when appetite disappears—ice chips, moist cloths, and humidifiers prevent distress from dry lips and airways. Position changes every few hours reduce pressure sores; blankets provide warmth as body temperature drops, though overheating must be avoided. These seemingly small gestures carry immense weight, transforming clinical observation into tender care.
Emotional support flows through gentle speech, soft music, and hand-holding, even when consciousness fades. Avoid correcting confusion or dismissing hallucinations; instead, listen without judgment and remain present without demanding engagement. The dying need permission to withdraw, not encouragement to fight the process.
Managing common symptoms—difficulty swallowing, incontinence, labored breathing—requires patience and practical solutions. Incontinence products maintain dignity; elevating the head eases breathing; a humidifier soothes rattled airways. None of these interventions cure, but all acknowledge suffering and respond with respect.
Caregiver burnout is a silent threat demanding equal attention. Support groups, grief counselors, professional caregivers, and regular breaks aren’t luxuries—they’re necessities for maintaining emotional resilience. Self-care isn’t indulgent; it’s essential for sustaining the presence your loved one needs.
End-of-life care ultimately honors both the dying and those who remain. Through balanced compassion for patient and self, you transform an inevitable passage into a meaningful farewell.