📌 Tick bites: how they can trigger a red meat allergy without you knowing it

Posted 16 January 2026 by: Admin
The Invisible Danger Of Tick Bites: Beyond Lyme Disease
Most people bitten by a tick follow a reassuring ritual: removal of the arachnid, disinfection, then back to normal. However, this approach minimizes a concerning reality that infectious disease experts have been documenting for years.
Unlike mosquitoes that bite and disappear in seconds, ticks anchor themselves in the skin and feed for 24 to 72 hours. During this microscopic feast, they inject their saliva into their host’s blood while sucking up body fluids. This bidirectional exchange creates a fearsomely efficient transmission vector for a multitude of pathogens.
The discretion of these arachnids heightens the danger. Their bites are generally painless thanks to natural anesthetic compounds, allowing ticks to feed undetected. Victims often discover the presence of the parasite during a shower or by pure chance, sometimes after several days of exposure.
But the threat doesn’t stop at known bacterial infections like Lyme disease. Recent research reveals that tick bites trigger aberrant immune responses, neurological dysfunctions, and metabolic upheavals whose manifestations may not appear until years after the initial incident. Some people develop debilitating chronic symptoms without ever establishing the link to this forgotten bite.
This ability to simultaneously carry multiple pathogens transforms every bite into a biological lottery with unpredictable and often irreversible consequences.
Alpha-Gal Syndrome: The Mysterious Allergy That Turns Meat Eaters Into Allergy Sufferers
This cascade of immune reactions can lead to a consequence as surprising as it is disabling: alpha-gal syndrome, a food allergy that arises without warning and radically disrupts one’s relationship with food.
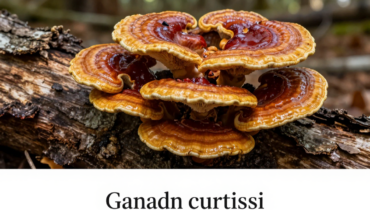
Alpha-gal refers to a sugar molecule (galactose-α-1,3-galactose) present in most mammals, with the notable exception of humans and primates. When certain ticks, primarily the Lone Star tick but also other species, bite an individual, they introduce this foreign molecule into the bloodstream. In response, the body produces antibodies against alpha-gal, making the person allergic to mammalian meat.
Victims suddenly develop reactions to beef, pork, lamb, game, gelatin, and sometimes dairy products. The phenomenon strikes regardless of age, even affecting people who have consumed meat daily for fifty years without the slightest problem.
The cruelty of this condition lies in its unpredictable nature. Unlike classic allergies that manifest in minutes, alpha-gal syndrome reactions occur three to eight hours after ingestion. This deceptive timing transforms every meal into medical Russian roulette: a steak enjoyed at dinner causes hives, swelling, and respiratory distress in the middle of the night, when no one thinks to blame the food.
Some patients present only violent digestive symptoms, others skin or respiratory manifestations, making clinical patterns difficult to identify for uninformed healthcare professionals.
Why This Allergy Evades Medical Diagnosis For Years
This delayed timing explains why so many patients wander from one doctor’s office to another without getting an answer. The three-to-eight-hour delay between consumption and symptoms creates a diagnostic blind spot that even experienced professionals struggle to identify.
Clinical manifestations vary considerably from person to person. Some develop unexplained chronic hives, others suffer from violent abdominal cramps, persistent bloating, or recurrent diarrhea. The most serious cases present swelling of the lips, tongue, and throat, which can lead to anaphylaxis. This symptomatic diversity misleads doctors looking for a consistent clinical picture.
Misdiagnoses multiply: irritable bowel syndrome, chronic hives, anxiety disorders, gastroesophageal reflux. Patients undergo batteries of tests, inappropriate treatments, and repeated consultations, accumulating frustration and discouragement. Some eventually believe their symptoms are psychosomatic.
The major obstacle lies in standard allergy tests which never include alpha-gal unless explicitly requested. Without a known tick bite history—and many go unnoticed—practitioners simply do not think of this possibility. The widespread lack of awareness of alpha-gal syndrome in the medical community, particularly in regions where tick awareness remains low, perpetuates years of diagnostic wandering.
The inconsistency of reactions further complicates the picture: symptoms sometimes only appear after consuming fatty meats, post-meal exercise, or alcohol. This unpredictability transforms eating into a source of permanent anxiety, long before a diagnosis is even made.
Rise Of The Phenomenon And Essential Protection Strategies
Environmental factors largely explain this alarming progression. Climate change allows ticks to survive in formerly inhospitable territories, prolonging their activity period and expanding their range. Urban expansion into wooded areas multiplies contacts between humans and arachnids, while deer and rodent populations—preferred hosts for ticks—thrive without sufficient natural predators.
Beyond statistics, the psychological and social repercussions of alpha-gal syndrome profoundly disrupt patients’ lives. Anxiety before every meal becomes chronic, the fear of accidental exposure omnipresent. Restaurant outings turn into ordeals, family invitations into sources of stress. Food, anchored in cultural traditions and childhood memories, suddenly becomes a threat. This break with foods consumed for decades creates a sense of identity loss that is difficult to express.
Prevention remains the only effective shield. Outdoors, prioritize long clothing, pants tucked into socks, and repellents containing DEET or permethrin. After every outing, thoroughly inspect your body and that of your animals, shower within two hours, and wash your clothes at high temperatures. Around your home, mow regularly, eliminate leaf piles, and create gravel barriers.
If a tick bites you, remove it with tweezers, disinfect carefully, and document any unusual symptoms during the following weeks and months. Systematically mention this bite during future consultations, even years later. Vigilance today can save years of unexplained suffering tomorrow.