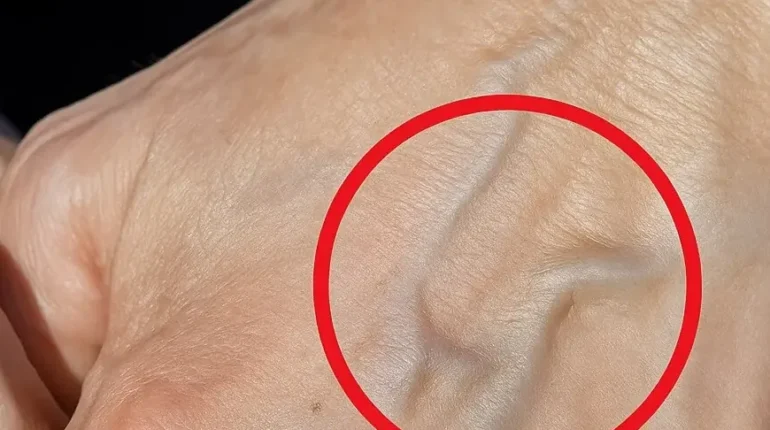
📌 Visible veins: When sudden appearance signals thrombosis or liver disease beyond cosmetic concerns
Posted 10 December 2025 by: Admin
Understanding Why Veins Suddenly Become Visible
Bulging veins appearing without warning often trigger unnecessary alarm, yet most cases stem from entirely benign causes. The human body responds predictably to everyday stressors—intense exercise, rising temperatures, aging, tight clothing, and genetics all prompt veins to become more prominent. Sun exposure and weight fluctuations similarly influence how visible your vascular system appears beneath the skin.
The mechanics behind this visibility are straightforward: veins bulge when blood pools in weakened or damaged veins, disrupting the smooth return flow to the heart. This pooling effect frequently results in varicose veins—swollen, twisted vessels that typically manifest on the legs but can develop on the arms as well. Understanding this distinction matters. A temporary prominence after a demanding workout or during hot weather differs fundamentally from persistent swelling accompanied by discoloration or pain.
Most visible veins represent a cosmetic or temporary adaptation rather than a medical emergency. Your body’s vascular system adjusts continuously to environmental and physical demands. However, sudden or unexplained changes warrant closer examination. The challenge lies in discerning between routine visibility and symptoms suggesting underlying vascular compromise. Recognizing this spectrum—from harmless adaptation to potential concern—empowers you to distinguish what requires immediate attention from what simply reflects natural bodily responses.
Medical Conditions Behind Prominent Veins
When visible veins persist beyond temporary circumstances, underlying medical conditions often deserve consideration. Three primary vascular conditions can trigger abnormal prominence: phlebitis causes inflammation within veins, producing tenderness and localized swelling that distinguishes it from simple visibility. Varicose veins represent a more chronic presentation—enlarged, twisted vessels that develop when valve dysfunction allows blood to pool rather than circulate efficiently back toward the heart. These may accompany discomfort ranging from mild aching to significant pain.
More serious conditions warrant heightened attention. Deep vein thrombosis involves blood clot formation, typically in leg veins, representing a medical emergency requiring immediate intervention. While less common, upper body vein prominence occasionally signals complications involving internal organs, particularly the liver or cardiovascular system. These rare presentations emphasize why sudden changes demand professional evaluation rather than assumption.
The distinction matters profoundly. Temporary visibility following exercise or heat exposure resolves naturally within hours. Persistent prominence accompanied by swelling, discoloration, warmth, or pain indicates something more complex occurring beneath the surface. Your vascular system communicates through these physical changes—learning to interpret these signals determines whether intervention prevents serious complications or unnecessary worry clouds routine adaptations.
Critical Warning Signs That Demand Attention
While most visible veins resolve naturally, certain symptoms signal conditions requiring immediate medical consultation. Swelling or pain in the limbs accompanying vein prominence suggests blood flow obstruction rather than cosmetic changes. Skin discoloration—ranging from pale patches to darkened areas near affected veins—indicates prolonged circulation problems affecting surrounding tissue health.
Warmth or redness over the affected area represents another critical indicator. These signs suggest inflammation or potential clot formation rather than simple vein visibility. Equally important are unusual vein patterns appearing on the chest or abdomen, which rarely occur from exercise or temperature fluctuations and may reflect internal pressure changes affecting deeper vascular systems.
The timeline matters significantly. Veins appearing suddenly without preceding activity, environmental triggers, or clear causation warrant investigation. When multiple warning signs cluster together—swelling combined with discoloration, or pain alongside unusual patterns—the probability of underlying pathology increases substantially. Your body seldom presents multiple vascular changes simultaneously without reason.
Distinguishing routine visibility from genuine concern hinges on these markers. Temporary bulging after workouts dissipates within hours, leaving no residual symptoms. Persistent changes accompanied by physical discomfort or appearance modifications demand professional evaluation. Recognizing these distinctions empowers informed decisions about whether observation suffices or intervention becomes necessary.
When Professional Medical Evaluation Becomes Essential
The distinction between harmless visibility and concerning changes ultimately rests on one fundamental question: does your vein prominence demand professional assessment? Veins appearing without clear reason—absent recent exercise, temperature exposure, or other identifiable triggers—represent the first indication that evaluation warrants consideration. This unexplained emergence signals potential underlying circulatory or systemic issues deserving expert examination.
Pain, cramping, or swelling accompanying vein changes elevate urgency considerably. These symptoms suggest blood flow disruption rather than cosmetic adaptation, indicating your body requires medical investigation. Similarly, observable changes in skin color or texture surrounding affected veins—whether lightening, darkening, or textural shifts—reflect circulatory compromise affecting dermal health and demand professional assessment.
The psychological dimension merits equal consideration. Seeking professional consultation for peace of mind represents entirely legitimate healthcare decision-making. Uncertainty about your body’s signals creates unnecessary anxiety that qualified evaluation efficiently resolves. A brief medical consultation either confirms benign changes or identifies conditions requiring intervention, transforming ambiguity into actionable knowledge.
Ultimately, understanding your body’s signals and respecting what they communicate defines proactive health stewardship. Most visible veins result from ordinary physiological adaptation to activity, temperature, or age progression. Yet when changes feel unexplained, produce discomfort, or simply generate concern, professional guidance transforms uncertainty into confidence. Your healthcare provider stands ready to distinguish routine changes from genuine medical considerations.