📌 Here’s the reality about diabetes symptoms doctors rarely explain upfront

Posted 7 December 2025 by: Admin
Understanding Diabetes: When Your Body’s Energy System Fails
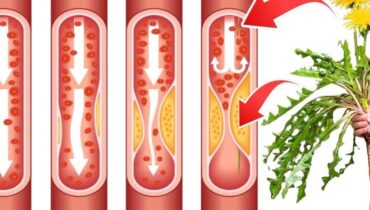
Diabetes represents far more than a simple metabolic hiccup. This chronic condition fundamentally disrupts how your body processes glucose, the primary fuel that powers every cell. Rather than entering cells efficiently, excess sugar accumulates in the bloodstream, initiating a cascade of damage across multiple organs over time.
What makes diabetes particularly insidious is its silent progression. Many people live with diabetes for years without realizing it, because the signs may at first seem mild or easy to ignore. This delayed recognition stems from the condition’s gradual onset and the tendency to dismiss early warning signs as normal aging or temporary fatigue. The body doesn’t announce its struggle loudly—it whispers through subtle shifts in thirst, energy levels, and bathroom habits that countless individuals overlook or attribute to other causes.
Understanding the mechanism behind these symptoms proves essential for early detection. When blood sugar remains elevated without proper cellular absorption, a physiological chain reaction begins. The kidneys detect this excess and attempt to filter it out, triggering a cascade of bodily responses. This mechanism explains why seemingly unrelated symptoms—from persistent thirst to unexplained weight loss to blurred vision—all stem from the same underlying problem.
The window for intervention narrows as diabetes progresses unchecked. Recognizing these early manifestations before permanent organ damage occurs separates those who manage the condition effectively from those who face severe complications. The pathway to diagnosis begins with understanding what your body is actually trying to communicate.
The Most Common Warning Signs: Thirst, Urination, and Unexplained Changes
The physiological chain reaction triggered by elevated blood sugar manifests first through symptoms most people attribute to everyday stress or seasonal changes. Frequent urination, particularly at night, stands as one of the earliest red flags. When glucose concentrations exceed the kidneys’ reabsorption capacity, these organs initiate a desperate filtration strategy—they expel excess sugar into the urine, but this process extracts water along with it, forcing more frequent bathroom visits and disrupting sleep patterns.
This mechanism directly produces the second hallmark symptom: excessive thirst that persists regardless of fluid intake. As the body sheds water through increased urination, dehydration triggers an unquenchable thirst cycle. You drink, yet the thirst returns quickly because your system remains locked in its struggle to eliminate the surplus glucose. This dual manifestation—urinating more while feeling perpetually parched—often occurs simultaneously, yet individuals frequently interpret these as separate, unrelated issues.
Simultaneously, affected individuals experience intensified hunger despite consuming normal or even elevated food amounts. Because glucose fails to penetrate cells efficiently, the body perceives starvation at the cellular level. It signals urgency for more fuel, even as adequate nutrition enters the digestive system. This creates a paradox: eating more while feeling increasingly unsatisfied.
Accompanying this metabolic confusion, many experience unexplained weight loss, particularly those with type 1 diabetes. When cells cannot access glucose for energy, the body initiates metabolic desperation—breaking down fat and muscle reserves to survive. Weight drops without intentional dieting, a seemingly positive change that masks profound internal struggle. These interconnected symptoms form a recognizable pattern that, once identified, demands immediate medical evaluation.
Beyond Metabolism: How Diabetes Affects Vision, Energy, and Healing
While the metabolic cascade dominates early diabetes progression, untreated high blood sugar extends its damage far beyond glucose regulation, systematically compromising multiple organ systems. The consequences ripple outward invisibly until they become impossible to ignore.
Fatigue emerges as a relentless companion when cells deprived of glucose cannot generate sufficient energy. Unlike ordinary tiredness that resolves with rest, this exhaustion persists after full nights of sleep, eroding work performance, concentration, and emotional resilience. The body essentially starves at the cellular level, running on reserve fuel that cannot sustain normal function.
Vision begins deteriorating through a deceptively subtle mechanism. High blood sugar alters the fluid balance within eye lenses, causing blurred vision that initially appears intermittent and easily dismissed as aging or screen fatigue. This temporary blurriness masks progressive danger—prolonged hyperglycemia damages the delicate blood vessels nourishing the retina, potentially triggering irreversible blindness if left untreated.
The circulatory compromise becomes evident through impaired wound healing. When elevated glucose damages blood vessels and restricts oxygen flow to tissues, cuts and injuries resist normal recovery. Simultaneously, the immune system’s weakened response creates vulnerability to recurring infections—skin conditions, gum disease, urinary tract infections—that respond poorly to treatment.
Perhaps most insidious is peripheral neuropathy: tingling, burning, or numbness spreading through hands and feet as prolonged high blood sugar corrodes nerve fibers. Initially subtle, this nerve damage can advance toward permanent dysfunction and chronic pain without intervention.
These cascading complications underscore a critical truth: diabetes rarely announces itself through a single dramatic symptom. Instead, it progresses silently through interconnected warning signs that demand recognition.
Nerve Damage And The Importance Of Early Diagnosis
The nerve damage that develops alongside diabetes represents one of the condition’s most insidious long-term threats. Peripheral neuropathy—manifesting as tingling, burning, or numbness in the hands and feet—occurs when prolonged elevated blood sugar systematically destroys nerve fibers. Initially mild and easily dismissed, these sensations can progress to permanent dysfunction and chronic pain without intervention.
What makes diabetes particularly deceptive is its variable presentation. Type 2 diabetes evolves so gradually over years that many people remain unaware of their condition entirely. Some individuals experience no noticeable symptoms whatsoever, discovering diabetes only during routine blood work. This delayed detection carries profound consequences: by the time diagnosis occurs, significant organ damage may already have commenced.
This reality underscores why regular screening becomes non-negotiable for at-risk populations. Those carrying risk factors—obesity, family history of diabetes, elevated blood pressure, or sedentary lifestyles—face substantially elevated vulnerability. A single blood test can reveal what years of subtle symptoms could not: the presence of a condition that, once identified, becomes manageable through proper medical intervention.
Early diagnosis fundamentally alters the trajectory of diabetes. Recognizing the condition before complications become irreversible allows individuals to implement lifestyle modifications and medical treatments that prevent blindness, kidney failure, amputation, and heart disease. The difference between catching diabetes in its early stages and discovering it years later, already burdened by complications, is the difference between disease management and survival.